Project Partners





Cervical cancer is the second commonest cancer of the female reproductive system in Nigeria but the commonest female cancer in Sub-Saharan Africa as a whole. World Health Organization (WHO) and other agencies currently recommend HPV test-based screening globally, but these tests are still too expensive for routine use in Sub-Saharan African countries. In recent years, Artificial Intelligence (AI) augmented mobile colposcopy built into the framework of mobile phones that are widely available in Sub-Saharan African (SSA) countries have become available. These technologies offer new opportunities for potentially more cost effective, cervical cancer screening that can be implemented by non-specialists and do not require extensive infrastructure which is very limited in Africa.
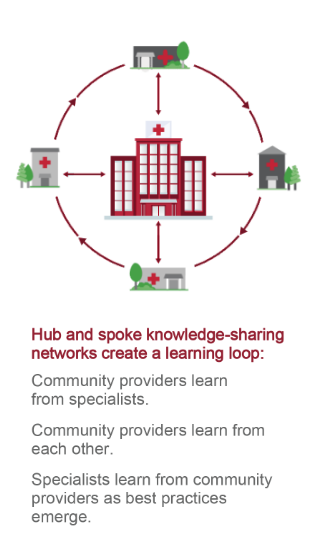
 The Extension for Community Healthcare Outcomes (ECHO) program was created at the University of New Mexico in 2003 to build provider capacity in hepatitis C treatment in underserved communities. It takes advantage of proven adult learning techniques and interactive video technology (the ECHO Model™) to connect groups of community providers with specialists at centers of excellence in regular real-time collaborative sessions. The sessions, designed around case-based learning and mentorship, help local workers gain the expertise required to provide needed services. Providers gain skills and confidence; specialists learn new approaches for applying their knowledge across diverse cultural and geographical contexts. The outcome is improvement in the capacity of the local workforce leading to improvement implementation of interventions and health outcomes.
The Extension for Community Healthcare Outcomes (ECHO) program was created at the University of New Mexico in 2003 to build provider capacity in hepatitis C treatment in underserved communities. It takes advantage of proven adult learning techniques and interactive video technology (the ECHO Model™) to connect groups of community providers with specialists at centers of excellence in regular real-time collaborative sessions. The sessions, designed around case-based learning and mentorship, help local workers gain the expertise required to provide needed services. Providers gain skills and confidence; specialists learn new approaches for applying their knowledge across diverse cultural and geographical contexts. The outcome is improvement in the capacity of the local workforce leading to improvement implementation of interventions and health outcomes.
To date, the ECHO program has been applied to therapeutic interventions, e.g. empowering providers to treat patients with Hepatitis C. While these approaches have achieved tremendous successes, adaptation of the ECHO model for implementation of early detection and prevention is likely to lead to even greater population health benefits. Cervical cancer screening methods implemented in large number of healthcare settings in SSA is particularly suitable for the ECHO model.
Cervical cancer has a long prodromal phase, characterized by progressive cervical intraepithelial neoplasia (CIN2+) which can be detected colposcopically in < 5% of women. The tests for CIN have high specificity and can exclude women at very low risk. Women with CIN2+ can be treated while those with more extensive lesions are referred. In Nigeria, AI-augmented mobile colposcopy (AVE) is being adopted for cervical cancer screening. In addition to the AI-augmentation, the mobile colposcope offers opportunity for remote tele-colposcopy, expert consultation and mentoring which will substantially increase the value of this technology in SSA.
In the Nigeria UNM UMB Cancer Control ECHO (NUUCCE) Program, we adopt and adapt the ECHO Model and implement it to build capacity of nurse-colposcopists to implement cervical cancer screening in Nigeria. We frame the implementation of the ECHO Model using the Consolidated Framework for Implementation Research (CFIR) framework and measure implementation outcomes using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework.